Celiac Disease — What it is, what it isn’t, why it’s important to know the difference.
Celiac disease (also known as celiac sprue, coeliac disease, non-tropical sprue or gluten sensitive enteropathy) is a chronic and permanent sensitivity to the food protein gluten, found in the grains wheat, barley, rye and triticale (a rye-wheat blend).
Who Gets Celiac Disease?
If you think you know the kind of person who might have celiac disease, you’re probably wrong. It can happen to just about anyone, no matter their ethnic or geographic background. Approximately 1% of any population group has it, although also having certain other diseases increases your risk.
Celiac disease occurs in children, women and men of all ages and it anyone with the right (or wrong, as it were) genes can develop the disease. It is the most common genetic disorder in North America and Europe, and is found in populations all over the world. In fact, the population with the highest prevalence of celiac disease is the Sahrawi population of North Africa (5.6%).
Celiac disease is an autoimmune disease, meaning the body attacks itself in an inappropriate immune system reaction. In this case, the reaction is to exposure to gliadin, a protein of the food molecule gluten, which is found in wheat, barley and rye.

In most all other autoimmune diseases, the catalyst for starting the body’s inappropriate reaction is not yet known. Celiac disease is unique in that it is the only autoimmune disease for which we know the trigger and therefore we can stop it: completely eliminate gluten from your diet.
Want to know HOW to eliminate gluten from your diet and from your life? Hop to my article, 7 First Steps to Going Gluten Free.
Why Early Detection and Diagnosis of Celiac Disease is Important
It’s critical to properly diagnosed if you have celiac disease, and to get diagnosed early. Like other autoimmune diseases, the longer your body suffers with active celiac disease, the more likely you are to also begin to suffer from other conditions like those outlined below, and the more likely you are to develop additional autoimmune diseases. We know that celiac disease prevalence increases from approximately 1% in the general population to between 5-20% prevalence in those with first-degree relatives with celiac, those with Type 1 Diabetes Mellitus (T1DM), chronic diarrhea, failure to thrive, Down syndrome, Turner syndrome, autoimmune thyroiditis, selective IgA deficiency, and William syndrome.
This fact bears repeating: even if you don’t think the symptoms of celiac disease you may be suffering are worth paying attention to now, the mere fact that you or a family member have been diagnosed puts you at a higher risk for developing another autoimmune disorder, while following a gluten-free diet (GFD) actually has a protective effect against contracting additional autoimmune diseases. The flip side is that early diagnosis of celiac disease with gut healing due to following a gluten-free diet may actually decrease the risk to develop secondary inflammatory bowel diseases.
Italy is perhaps the most forward-thinking when it comes to celiac testing, as it requires screening for celiac as well as Type 1 diabetes in the entire population, aged 1-17. This law was passed in 2023. No other country has similar requirements, although testing when symptoms or family history are present just makes sense.
Nearly all ACTIVE autoimmune diseases decrease life expectancy. Autoimmune diseases include celiac disease, rheumatoid arthritis, Lupus, Type 1 Diabetes, multiple sclerosis, Inflammatory Bowel Disease (IBD) including Crohn’s Disease and Ulcerative Colitis, Addison’s Disease, Graves’ Disease, Sjögren’s syndrome, Hashimoto’s thyroiditis and others. None of these is something anyone would aspire to contract; if you could avoid them, you would, wouldn’t you?
How Does Celiac Disease Work?
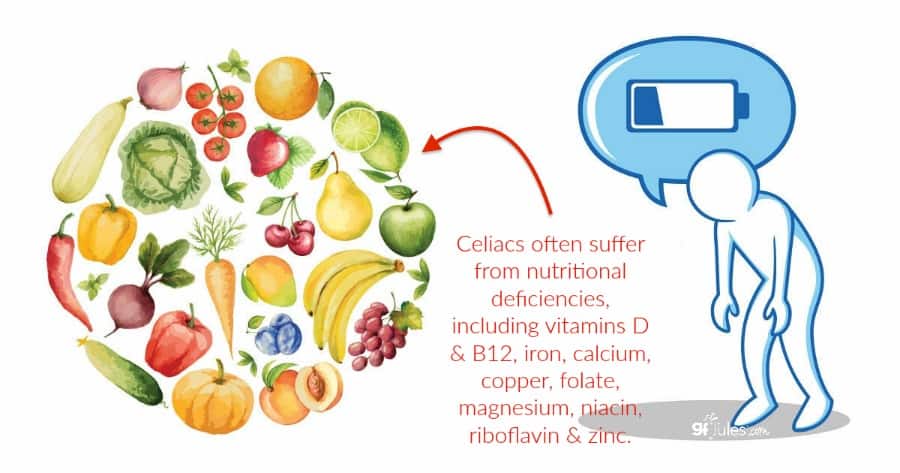
Because of the way celiac affects the gastrointestinal tract, it affects the body’s ability to properly absorb nutrients. Continued exposure to gluten leads to continued damage of the small intestine (more on that, specifically, below) leading to malabsorption of essential nutrients like iron, calcium, folate, vitamins A, D, E, and K, and protein, which ultimately leads to nutritional deficiencies including anemia and osteoporosis.
Further complications of untreated celiac disease can include infertility in both men and women and men, miscarriage, and lymphomas.
Once on a gluten-free diet, your body will begin to heal and you should be able to put the disease into remission, again, making you less likely to contract another autoimmune disease than if you had continued to eat gluten and perpetuated your active celiac disease.
How Soon Will My Body Heal from Celiac Disease?
A recent study sheds light on why many celiac patients fail to completely heal though, even on a strict gluten-free diet. Factors contributing to better healing include: younger age at diagnosis, less severe initial damage and being male. It is well accepted that diagnosed children in general recover more quickly than do adults, for whom the mean time to symptom relief is four to eight weeks.
A 2023 study devised a 5-point system to score celiac patients for the likelihood of risk for persistent intestinal damage, and therefore, need for follow up endoscopy. If patients were over 45 when diagnosed with celiac disease, exhibited “classic” gastrointestinal symptoms, respond poorly to the gluten free diet and/or don’t adequately follow the gluten free diet, they would be at the highest end of the risk scale and recommended for follow up biopsy due to the likelihood of persistent intestinal damage.
What Celiac Disease Does to the Body – an in-depth look.
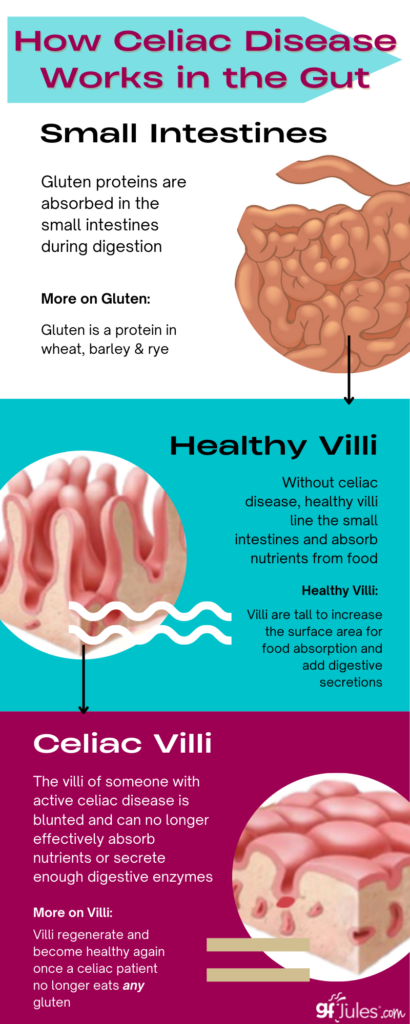
Celiac disease’s “reaction” is best explained with a review of the small intestines. In a normal, healthy person, the small intestine is lined with shag-carpet-like projections of tissue called villi. Your villi absorb valuable nutrients into your bloodstream. They also block the absorption of certain molecules.
Celiac disease makes these intestinal linings abnormally permeable, allowing some molecules, namely gluten, to be absorbed through the gut. Because this leakage allows gluten into areas it wouldn’t normally be allowed to, the body launches an immune assault against it. This assault causes an inflammatory reaction and damages the villi that have absorbed it.
Over time, through repeated absorption and the ensuing damage, these villi are blunted and flattened. This in turn destroys the body’s ability to properly absorb food. The result: intestines that can no longer efficiently or effectively absorb all kinds of nutrients from food. This damage begins a chain reaction in the body that may or may not produce noticeable symptoms.
The presence of symptoms can depend on how long someone’s body has been actively reacting to gluten, and on how their body presents physical symptoms. The only way to prevent this effect in a person with celiac disease is by adopting a life-long gluten-free diet. There is no magic pill other than avoiding gluten entirely.
But compared to any other auto-immune disease, knowing an antidote, so to speak, exists—in the form of a gluten-free diet—should give anyone diagnosed with celiac disease some measure of comfort.
Once a diagnosed celiac patient removes gluten from their diet entirely, their villi will begin to heal, as the intestine renews itself every three days. The amount of time it will take the intestine to fully recuperate once no longer exposed to gluten varies with the individual.
Celiac Disease, Wheat Allergy, Gluten Sensitivity: What’s the Difference?
Celiac Disease is often inaccurately equated with other, very different conditions.
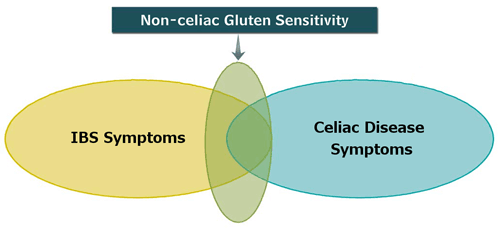
Gluten sensitivity and wheat allergy sometimes mimic celiac disease symptoms. They’re also treated with a gluten-free diet. But these conditions are quite different from celiac disease. That’s why it’s important to accurately diagnose which condition is causing your distress.
How Celiac Disease Differs from a Wheat Allergy.
An allergy to wheat is actually very different from celiac disease. A wheat allergy is not an autoimmune disorder at all. Rather, it is someone’s body mistakenly thinking the wheat’s food protein is a true pathogen. So, while you would normally be happy when your body creates antibodies to fight a pathogen, it instead wages war on what, in most people, is a harmless food protein.
In full combat mode, your body attaches these newly created antibodies to the food molecule. This causes still other cells to join in the attack by releasing histamines. The body’s attack may produce a variety of symptoms, usually unique to the individual. Like most true allergies, these symptoms are often rapid and may be severe.
Food allergy symptoms can range from a skin rash to gastrointestinal distress, swelling, migraines or even difficulty breathing. Luckily, once the allergen is removed from the body, or in many cases, if the person takes antihistamines, the body can quickly get back to normal. This rebound differs greatly when compared to the often long-term effects gluten produces in someone with celiac disease.
How Celiac Disease Differs from Gluten Sensitivity.
While not an autoimmune disease like celiac disease, “Gluten Sensitivity,” or “Non-Celiac Gluten Sensitivity” (NCGS) is also relieved by eating a gluten free diet. These food intolerances occur when someone’s body can’t metabolize certain foods. This inability typically is caused by a lack of certain enzymes needed to break down particular food components.
People with gluten sensitivity often have many of the same symptoms celiac disease can produce. The difference is that they test negative for celiac disease by bloodwork and endoscopy (there is currently no accepted test to diagnose NCGS). But through trial and error, people with gluten sensitivities learn that gluten is the cause of their discomfort.
Once their gluten-free diet relieves their symptoms, these self-diagnosed people can quickly get back to feeling good and living happy, healthy lives. Unfortunately, without a hard-and-fast celiac disease diagnosis, these people’s decisions to eat gluten free are questioned.
Worse, they’re ridiculed or not taken seriously by the people sometimes responsible for safeguarding their meals. Most unfortunate is when they are lumped into a population that has joined ‘the gluten free fad,’ a term arising from the gluten free movement’s tremendous growth, and its increasingly high visibility in the news (in serious reports as well as many that seek to de-value it and make fun of those who genuinely feel better avoiding gluten).
For more information on NON-Celiac Gluten Sensitivity, go here.
How Do I Know if I Have Celiac Disease?
Celiac disease can, unfortunately, create years of unexplained symptoms. That’s because an unhealthy intestinal tract can affect virtually every other system in the body. It’s one of the reasons celiac symptoms are often so difficult to distinguish from the symptoms of many other conditions.
“There is a large proportion of the population that has the disease without knowing it, either because they don’t have symptoms yet, or the symptoms are so vague they don’t pay attention to it,”
One person may have an unexplained history of migraines, someone else of arthritis and yet another of chronic fatigue or thyroid problems. Up to 40 percent of people with celiac disease do not have typical gastrointestinal complaints. As different as the symptoms are, all may later discover the root cause has been untreated celiac disease.
This wide range of symptoms is a great illustration of why it still takes an average of 6 to 12 YEARS from the first symptoms to a medical diagnosis of celiac disease. At best, only one-quarter of those with celiac disease have actually been diagnosed by a physician. A whole-body approach to symptoms examination is the best way to begin to evaluate the potential for celiac or other conditions.
Testing for Celiac Disease
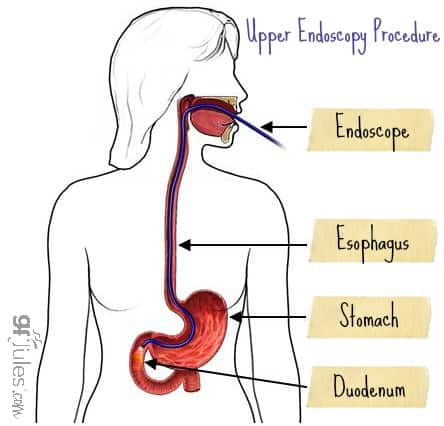
Fortunately, extremely accurate blood tests combined with an endoscopic biopsy can ultimately yield a firm, positive diagnosis of celiac disease.
According to the latest study, “nonbiopsy diagnosis may be considered only in HLA-DQ2.5/DQ8-positive individuals with both TG2-IgA and DGP-IgG serum titers above 10 times the upper normal limit (≥ 70 U/mL), as it otherwise may include patients with potential CD. Biopsy verification remains, therefore, the diagnostic gold standard for the majority of adult individuals with suspected CD.”
Regarding these blood tests, here is the latest on what is recommended (print this information and take to your doctor, if necessary, to make sure the right tests are run):
“Overall, the best serologic test for celiac disease is currently tissue transglutaminase (tTG)-IgA, which has a high sensitivity and specificity for untreated celiac disease, especially in high-risk groups. …. More nuanced approaches to serologic tests, such as combining the highly sensitive tTG-IgA with endomysial antibodies, very high titer tTG-IgA, or serially positive tTG by radioimmunoassay, have a diagnostic accuracy that rivals that of traditional biopsy-based approaches. The recent European Society for Paediatric Gastroenterology Hepatology and Nutrition guidelines for children have a nearly 100% positive predictive value for celiac disease when anti-tTG is 10 times the upper limit of normal or higher, regardless of symptom status.” (JAMA 2017)
It is essential that you insist your doctor take at least 4-6 duodenal biopsies during the endoscopy procedure: this includes 2 from the duodenal bulb and 4 from the distal duodenum. The American Gastroenterological Association now recommends that 6 distal duodenal biopsy specimens are necessary for accurate diagnosis because duodenal villous atrophy can be patchy and easily missed if fewer biopsies are taken.
Determining whether celiac disease could be the root of your particular problems is a great first step. As you can see below, the partial list of potential symptoms of celiac disease is as long as it is varied. To complicate things still further, these symptoms can occur individually, or in combination with others; they can occur sporadically or constantly.
What is “The Celiac Iceburg”?
To add yet another wrinkle, the majority of people with undiagnosed celiac disease actually suffer no overt symptoms—but they’re still at risk for developing serious complications. Let me repeat this a different way: just because you have few or no symptoms of celiac when you eat gluten does not mean you are “less sensitive” or you have “outgrown” the disease. Neither of these scenarios is real.
If you have diagnosed celiac disease, you have it for life, and symptomatic or not, you are putting yourself at risk for a host of other health problems, other autoimmune diseases and even an early death if you continue to eat gluten.
Your body views gluten as a poison; do not take this lightly. This asymptomatic condition is sometimes called the “Celiac Iceberg.” Just as most of a real iceberg’s mass is unseen, hidden under the water, the majority of a celiac’s risks lie undetected when the person shows no symptoms.
There are Over 300 Possible Celiac Disease Symptoms, Including:
- anemia (low hemoglobin or hematocrit)
- autoimmune disorders like rheumatoid arthritis and lupus
- behavioral changes (can include depression, irritability, failure to concentrate)
- bloating and gas or distended abdomen
- bone or joint pain
- changes in appetite
- chronic diarrhea
- colitis
- collagen vascular disease
- constipation
- dermatitis herpetiformis (burning, itchy and blistering skin rash)
- delayed growth in children and delayed onset of puberty
- dizziness
- easy bruising
- failure to thrive in infants
- fatigue and lethargy
- fibromyalgia
- hair loss
- headaches
- hypoglycemia (low blood sugar)
- hyposplenism (underactive spleen)
- increased risk of infections
- infertility and miscarriage
- iron deficiency
- irregular or speedy heartbeat
- lactose intolerance
- liver disease
- lupus
- lymphoma (cancer of the lymph glands)
- malnutrition
- migraines
- missed menstrual periods
- mental fog
- muscle cramps
- nausea and/or vomiting
- neurological problems (including schizophrenia, ataxia and epilepsy)
- nosebleeds
- osteoporosis or osteopenia
- pale, foul-smelling, bulky and/or fatty stools that float
- pale skin
- seizures
- short stature
- shortness of breath
- Sjögren’s Syndrome
- some intestinal cancers
- thyroid disease (hyper or hypothyroidism)
- tingling or numbness in the hands and feet
- tooth discoloration or dental enamel defects/loss
- type 1 Diabetes
- ulcers inside the mouth (aphthous ulcers); oral lichen planus, glossitis; or geographic tongue
- vitamin or mineral deficiency
- weight loss/gain
Active Celiac Disease Inhibits Nutrient Absorption, Which Creates Other Health Issues
After reading through the long list of potential symptoms of celiac disease, it’s easy to underplay the effects caused by the damage to the small intestine it causes.
When the small intestine is damaged, the result is an impaired ability for the body to absorb nutrients, carbohydrates and fats. These absorption issues, in turn, lead to still others.

Untreated celiac disease ultimately leads to malnutrition, which can cause a host of other health problems. Malabsorption of calcium and vitamin D and K can cause osteopenia (reduced mineral content in bones) or even osteoporosis (progressive bone thinning and weakening).
Miscarriage and birth defects can arise due to poor nutrient absorption and other resulting problems. Failure to thrive in infants, short stature and delayed development in children occur when there is a serious lack of nutrition. Anemia is caused by poor absorption of iron or from folic acid and vitamin B12 deficiencies.
Further complications of untreated or ignored celiac disease include developing other autoimmune diseases, thyroid problems, reproductive health issues and even cancer. Studies have even shown an increased connection to disease like non-Hodgkins Lymphoma, and that the risk of dying from lymphoma is higher in people with celiac disease. To mitigate this risk of developing cancer, following a strict gluten-free diet is always advised.
Celiac disease, unlike food intolerances and allergies, causes severe intestinal damage and can lead to nutritional deficiencies, among other health conditions.
Unrelated to gastrointestinal symptoms, recent studies have also confirmed that celiac disease causes neurological damage, including reaction time deficits, anxiety and depression. Other population studies have shown that those living with celiac disease are also at increased risk of developing conditions like vascular dementia in older age.
The Medical Community’s Role in Diagnosing, or Ruling Out, Celiac Disease
Doctors, nurses, even dentists and hygienists must thoroughly understand and aggressively recommend testing for active celiac disease to prevent future complications. Many times, celiac disease is misdiagnosed as irritable bowel syndrome, anemia, chronic fatigue syndrome. It’s often misdiagnosed as intestinal infection and Crohn’s disease. Anyone suspected of suffering from these conditions, or unexplained symptoms from the list above, needs to insist that their doctor test also for celiac disease.
Imad Absah, M.D., a pediatric gastroenterologist at Mayo Clinic says that
“About 1 in 5 children with celiac disease has constipation, so patients with constipation outside the range of what is physiologically normal should be screened. Kids with iron deficiency anemia that’s not responding to treatment should be tested, and any concern about growth should be checked.
“We are doing better at screening because of the vigilance of providers, but it can still be seven or eight years before some children are diagnosed.“
A celiac test can simply be requested as part of an overall blood panel, and should be, in determining the root cause of someone’s health problem(s). A recent multi-facility study showed that when primary care physicians test patients exhibiting any of the variety of symptoms of celiac disease, the rate of diagnosis increases between 32-fold to 43-fold!
An early diagnosis is crucial to preventing serious consequences from untreated celiac disease. Given the near universal access most of us have to a celiac blood test, there’s little reason for anyone with undiagnosed health issues to not be tested.

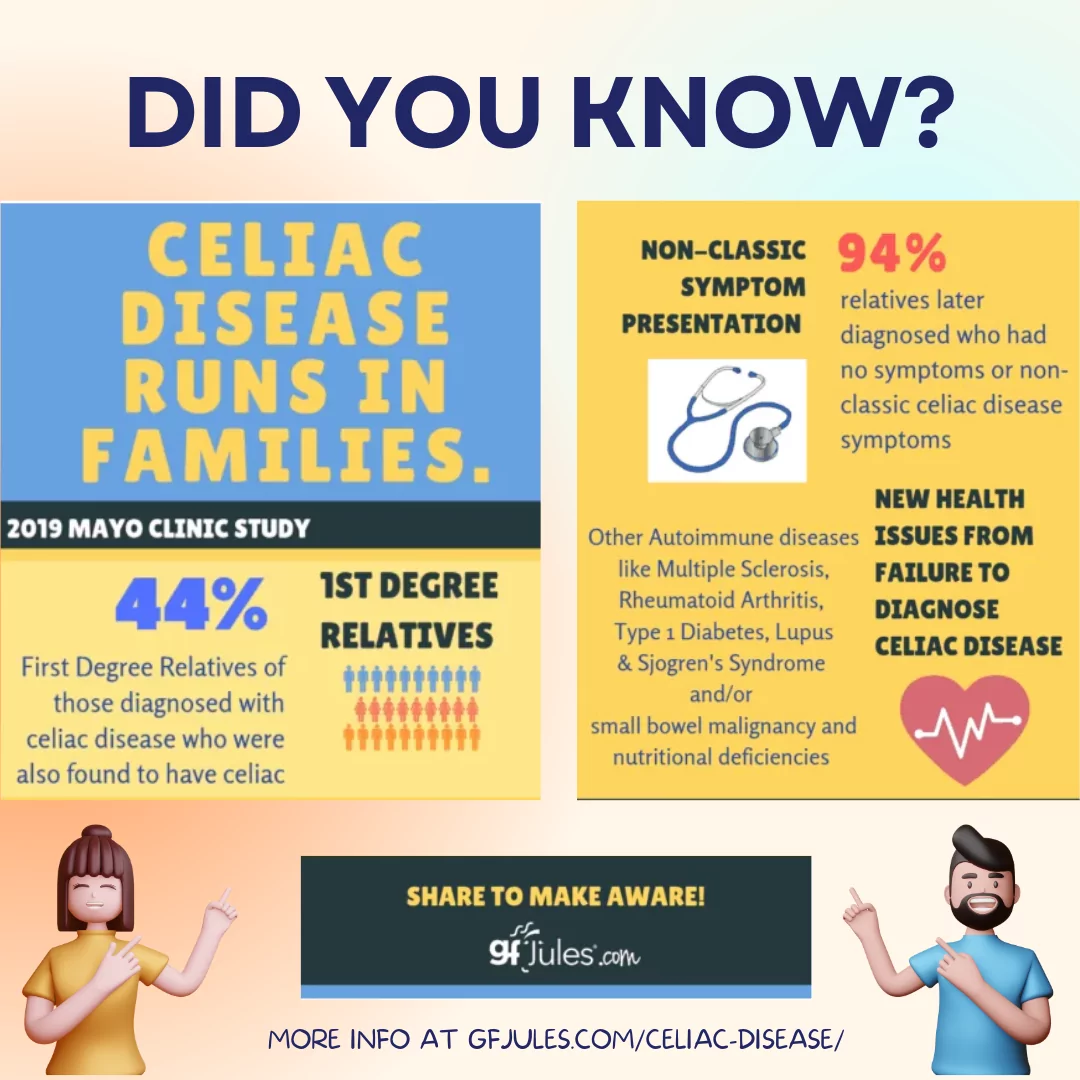
Furthermore, having a 1st-degree relative with celiac disease can greatly increase your risk of developing the disease. In fact, in a Mayo Clinic study, 44% of screened first-degree relatives of celiac patients had celiac disease! It is unlikely that many of those would have otherwise learned of their disease, since 94% of those had symptoms that were not classic or had no symptoms at all.
Current guidelines recommend that children with immediate family members who are celiac, or children with other risk factors like Type 1 diabetes, autoimmune thyroid disease, Down syndrome or Williams syndrome, should be screened for TTG antibodies around 3 years of age. Even if the child has no recognized symptoms, if he or she is high risk, antibody screening is recommended every one to three years until the age of 18, and every five years after that.
As you can see, it is crucial to understand the root cause of your problems with gluten. If you have medically diagnosed celiac disease, your physician must monitor your nutritional deficiencies. He or she must also look for signs of other autoimmune diseases or gastrointestinal cancers, in particular. What’s more, celiac disease is hereditary. Knowing whether or not you have it can help you decide if other family members should be tested to protect their health.
When one family member is diagnosed with celiac disease, first-degree relatives (a parent, child or sibling) have a 1 in 10 chance of also developing celiac disease; the risk drops to one in 39 for second-degree relatives (aunts, uncles, grandparents, etc.).
This point bears repeating: A 2019 study from the Mayo Clinic shows what we’ve been urging for years: Celiac indeed does run in families, so ALL FIRST DEGREE RELATIVES SHOULD ALSO BE TESTED. Nearly half of screened first-degree relatives of those diagnosed also were shown to have celiac disease. Of those patients almost none had “classic symptoms” or any symptoms at all, so would likely not have been tested otherwise.
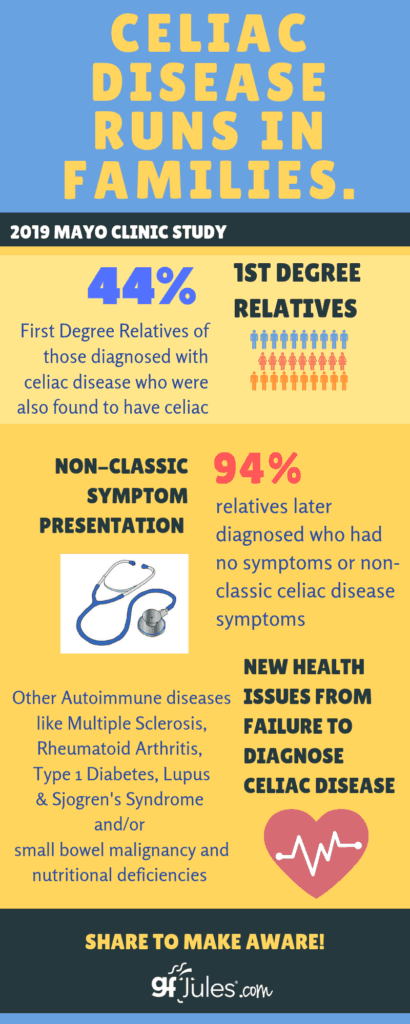
This kind of screening for celiac disease among family members could prevent other long-term complications like nutritional deficiencies, development of new autoimmune conditions (including Type 1 Diabetes, Lupus, Rheumatoid arthritis, Multiple Sclerosis, and Sjogren’s Syndrome), as well as small bowel malignancy.
There is now a genetic test which can rule out celiac for those without the specific genes HLA-DQ2 or DQ8. While the general population has a 1% chance of developing celiac (1 in 100 people), if you carry HLA-DQ2 and/or DQ8, your risk of developing celiac disease increases to 3%.
The genetic test is helpful to determine whether a person could develop celiac, although it does not determine if they will develop it or if they have it now. A surprising 30-40% of Americans have one or both of these genes, but the National Institutes of Health (NIH) reports that only 3% of those carriers will actually develop celiac disease.
Current recommendations are that the genetic test for celiac disease should be performed in asymptomatic 1st degree family members, especially children, in order to rule out the need for any future testing. Gene-positive 1st degree relatives should be tested for celiac disease every 3-5 years.
For more information, consult my book, The First Year: Celiac Disease and Living Gluten Free.

For Doctors and Other Medical Professionals Wanting to Know More About Celiac Disease and the Path to Diagnosis from the Patient’s Perspective
For several years, I’ve been honored to have been invited to speak at the University of Maryland School of Medicine about celiac disease from the patient’s perspective. I speak to the average diagnosis time (8-10 years) and the emotional and physical damage done by incorrect and delayed diagnoses. I describe both my own journey and the journeys of so many others who I’ve met in my travels across the country when I speak and through my work as a journalist, author and blogger.
I share about this annual lecture here in hopes that other medical schools adopt this forward-thinking approach and begin to ask the broader questions necessary to put celiac disease on the minds of tomorrow’s doctors in every field. Just think if an early and accurate celiac diagnosis could prevent the development of Type 1 Diabetes, Lupus, MS, thyroid disorders or cancer in even one patient.
We know that celiac affects 3 million Americans, at least 80% of whom remain undiagnosed. Where are these patients? Why are they being missed? There is a documented “undiagnosed burden” of celiac disease that can only be overcome through the work of physicians. Even when typical gastrointestinal symptoms don’t present — over half of adults with celiac have symptoms unrelated to the digestive track — it is incumbent upon physicians to look for this, one of the most common, yet still so undiagnosed, autoimmune diseases.

This year, I asked others to share some of their stories, successes and frustrations directly through Twitter and Facebook. I’ve linked the Facebook post here, and shared a few of the Twitter posts here as well.
The main message you need to take away from these personal anecdotes is that despite the improvement in testing and awareness, celiac disease continues to fly under the radar for most clinicians and remains incredibly under-diagnosed. Because it is an autoimmune disease, patients need an accurate diagnosis in order to take their treatment seriously and in order for (at least first degree) relatives to also get tested, regardless of the perceived seriousness or existence of overt symptoms.
“Celiac is not always textbook. If a mom brings you a kid with fatigue, anemia, depression, inflammation, joint pain, etc. Think gluten. Good chance this mom knows ‘something is not right w/her kid’.” @brenhouse208“From perspective of atty w/ CD, to not be afraid of reconsidering protocols since solely being GF healed me from skin, esophageal & colon cancers & 5 retina surgeries AND my Mom from Stage 4 NHLymphoma. Mom’s chemo was killing her so stopped, started GF & now 6 yrs cancer free” @EsqCGolfer“Tell their patients the long term consequences of cheating on a gluten free diet. I’ve never cheated once in a decade because I don’t want to deal with osteoporosis and cancer” @UndergroundEli1
“It’s not a ‘sensitivity’ or in our heads! Being ‘glutened ‘ is a real thing and we don’t do that on purpose!! Please understand we are confused, scared, depressed, and sometimes have been humiliated by our own body’s reaction when we have been ‘glutened’ in public.” @Lisa_Loyd
“Not everyone with celiac’s will realize that their stomach pain isn’t normal (I didn’t) because their stomach always has hurt, and may come in with a bunch of seemingly unrelated symptoms (peripheral neuropathy, joint pain, migraines, cupped nails, etc.).” @Andrea_HicksPhD
“Mostly that it’s more difficult to live a truly gluten free life than they might think. should be open and honest about complications patient might encounter and always refer to Celiac Specialist for accurate information.” @BeatCeliac
“That no matter what speciality – or type of practice they go into – they will encounter people with Celiac Disease. Also, a push for asking patients on intake if there’s a family history would be great too.” @BaltGF
“TFW patient gets when diagnosed, told to go gluten free, & released into the wild w/o nutritional or emotional support. Doctors need an educated nutritionist recommendation & support group/ other patients to guide newly diagnosed celiacs. Also connection 2 anxiety/depression” @MicBabay
“1. There is a link between celiac disease and mental health 2. Celiac patents often have other food allergies that prevent them from living their best life eg: Soy, Rice. Thank you for informing them of what it’s like.” @thequimbys1
“When diagnosing patients, refer them to an RD knowledgeable in #celiacdisease! Have a couple of RDs in their back pocket to refer them to!” @RachelBegunRD